Why Managing Behavioral Health Services is Essential for Modern Healthcare
Why is it important to manage behavioral health services? It is crucial for improving patient outcomes, lowering healthcare costs, and addressing the mental health crisis. When services are well-managed, patients receive integrated care that treats mind and body together, leading to better recovery and an improved quality of life.
Key reasons managing behavioral health services matters:
- Improved Patient Outcomes – Integrated care leads to better treatment results and faster recovery.
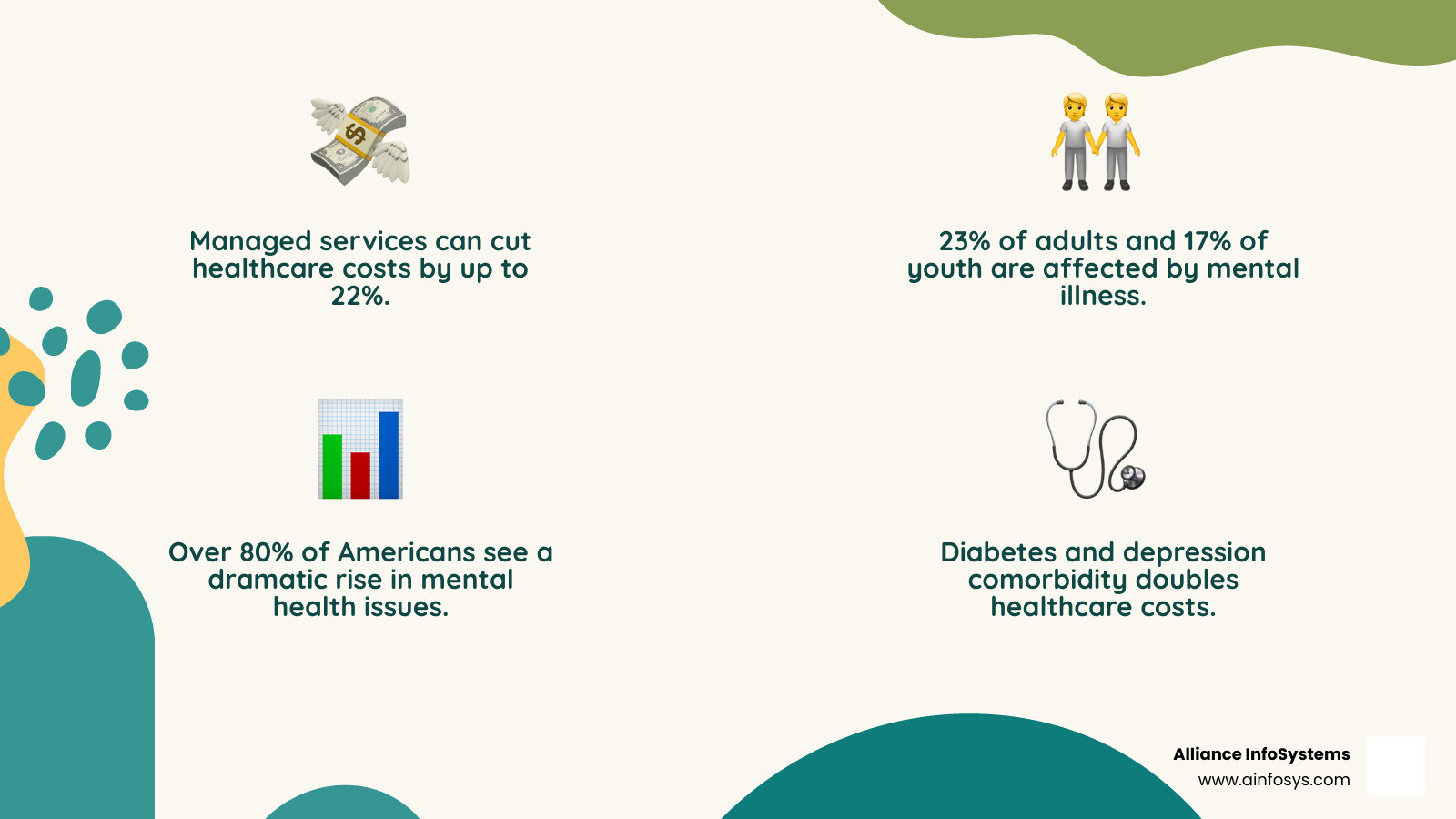
- Cost Reduction – Coordinated care can reduce healthcare costs by up to 22%.
- Increased Access – Well-managed services make mental health care more accessible.
- Provider Support – Collaborative care models reduce provider burnout.
- Population Health – Addresses mental illness affecting 23% of adults and 17% of youth.
Behavioral health—encompassing mental health, substance use, and life stressors—is too often treated separately from physical health. This fragmentation is a problem, especially as more than 80% of Americans perceive a rise in mental health issues. The mind-body connection is undeniable: people with diabetes are up to three times more likely to experience depression, and their combined healthcare costs more than double. Effectively managing behavioral health services means creating integrated systems that improve outcomes for patients while reducing costs and supporting providers.
The Critical Link: Understanding Behavioral Health and Its Overall Impact
To understand why it is important to manage behavioral health services, we must first grasp what behavioral health is. It’s an umbrella term covering mental health conditions like depression and anxiety, as well as the daily habits and stressors that affect our well-being, such as substance use, diet, and sleep. Its how our thoughts, feelings, and actions connect to our overall health.
Mental health is a state of well-being that allows us to handle lifes challenges and is shaped by personal, social, and economic factors. The need for effective management is clear: about one in five adults in the U.S. have a mental health disorder, according to SAMHSA, and many struggle to get treatment (see also NIMH statistics). The common overlap with substance use disorders (SUDs) makes managing these services essential for a healthy society.
The Unseen Connection: How Behavioral Health Governs Physical Health
The mind-body connection is a clinical reality. Untreated behavioral health conditions can manifest as physical symptoms, like anxiety causing stomachaches or depression leading to chronic pain, which drives up healthcare costs. This link, known as comorbidity, is common. For example, individuals with diabetes are up to three times more likely to experience depression. When these conditions coexist, annual healthcare costs can more than double. Beyond diagnoses, our behavioral health influences our sleep patterns, nutritional choices, and exercise habits. Neglected behavioral health can lead to stress-related illnesses and worsen chronic conditions.
Breaking the Silence: Addressing the Stigma Around Mental Healthcare
A major barrier to managing behavioral health is stigma, which creates a fear of judgment and discourages people from seeking help. This can lead to social isolation and worsening symptoms. Integrating behavioral health services into primary care is a powerful way to normalize conversation and reduce stigma. When a behavioral health professional is part of the regular doctor’s team, it signals that mental health is just as important as physical health. This model allows for “warm hand-offs,” where a patient is seamlessly connected to a specialist in the same visit. Along with public awareness campaigns, this approach helps create a society where seeking support for behavioral health is as natural as treating a broken bone.
Why Is It Important to Manage Behavioral Health Services Effectively?
Effectively managing behavioral health services optimizes our entire healthcare system. The positive ripple effects touch patients, providers, and the economy.
First, effective management leads to significantly improved patient outcomes. Integrated care helps people recover faster, develop healthier coping mechanisms, and enjoy a higher quality of life. The economic benefits are also substantial. Untreated behavioral health issues are costly, but integrated care models can lead to a 22% reduction in overall care costs. For older adults, coordinated care can decrease total costs by 10%. This shows that investing in behavioral health management is a financially sound choice that improves system efficiency. Finally, mentally healthy individuals contribute to increased workplace productivity, and integrated systems lead to higher job satisfaction and reduced burnout for providers.
The Power of Integration: Benefits for Patients and Providers
Integrating behavioral health into primary care is key to effective management, promoting “whole-person care.” For patients, this means earlier detection, as up to 70% of primary care visits are related to mental health. It also provides increased access to care in a familiar setting, reducing barriers like scheduling conflicts or stigma. For providers, integration improves their ability to treat patients with complex needs. Behavioral health specialists can offer consultations and help manage challenging cases, which boosts primary care physicians’ confidence and reduces provider burnout. Models like the Patient-Centered Medical Home (PCMH) and “warm hand-offs”—seamlessly transitioning patients to behavioral support during a visit—are powerful examples of how collaborative care teams empower both patients and providers.
Ensuring Equity: Addressing the Needs of Diverse Populations
A critical reason why it is important to manage behavioral health services is to ensure equitable access for all. Health inequities create unique barriers for many groups. An effective system must address these disparities:
- Children and Adolescents: Face a sharp increase in mental health conditions, with poverty and bias creating barriers to treatment.
- LGBTQ+ Individuals: Are 2.5 times more likely to experience depression, anxiety, and substance misuse, often facing discrimination in healthcare.
- Rural Populations: Suffer from a severe lack of specialists, with over 60% of rural Americans living in mental health shortage areas.
- Perinatal Mood Disorders: Affect one in five pregnant or postpartum individuals, yet 75% do not receive treatment.
- Older Adults: Are the least likely group to receive mental health treatment, facing unique challenges like social isolation and chronic illness.
- Racial and Ethnic Minorities: Bear a disproportionate burden of disability from mental illness due to barriers like a lack of culturally competent clinicians.
Addressing these disparities requires a commitment to culturally competent care, including universal screening and policies that promote equal access for everyone.
The Role of Technology in Modernizing Behavioral Health Management
Technology is a key part of answering why is it important to manage behavioral health services well. Digital tools are making care more effective, accessible, and patient-centered.
Telehealth and telepsychiatry have been game-changers, helping people in remote areas or with mobility issues access expert care. This digital change in healthcare allows providers to reach more patients. Electronic Health Records (EHRs) are vital for integrated care, allowing specialists to share information and coordinate treatment. Using data analytics, providers can track outcomes and identify trends to continuously improve care. Secure patient portals empower individuals to take an active role in their health.
At Alliance InfoSystems, our Managed IT Services provide the strong, dependable tech support behavioral health practices need, ensuring your systems run smoothly so you can focus on patients.
Why is it important to manage behavioral health services with robust IT security?
Behavioral health information is incredibly sensitive, which is why it is important to manage behavioral health services with strong IT security. Protecting patient privacy is a legal and ethical duty.
Compliance with regulations like HIPAA is mandatory. Violations can lead to heavy fines and a loss of patient trust. Healthcare is a prime target for cyberattacks, so protecting against data breaches and ransomware requires a proactive security strategy. System reliability is also crucial to prevent interruptions in care.
Alliance InfoSystems’ Managed Security Services are designed for healthcare’s unique needs, offering comprehensive protection for patient data. Our Data Backup and Recovery solutions ensure your vital data can be restored quickly after any incident, minimizing downtime. Furthermore, secure communication tools are essential for protecting patient privacy during telehealth sessions.
Expanding Access and Efficiency Through Digital Tools
Technology also makes behavioral health services more available and efficient. Telemedicine overcomes geographical barriers, especially in rural areas, making care more equitable. Digital tools also boost patient engagement. Mobile health apps can offer self-help resources, mood tracking, and easy communication with care teams, empowering patients in their treatment. For providers, EHR integration reduces administrative work, freeing up time for patient care. Flexible IT systems are crucial, and our Cloud & Virtualization Services provide the scalability and cost-efficiency modern practices need, allowing for secure, remote access to data and systems.
Navigating Challenges and Shaping the Future of Behavioral Healthcare
Even with our understanding of why it is important to manage behavioral health services effectively, significant roadblocks remain. Key challenges include a severe provider shortage, payment model reform, system fragmentation, insurance coverage gaps, and a lack of interoperability between IT systems.
Overcoming Systemic Problems in Service Delivery
These systemic problems are solvable. The workforce shortage is critical, as many primary care physicians struggle to connect patients to mental health services. Solutions include expanding the roles of existing professionals. Financial barriers like inadequate reimbursement also persist. Hope lies in new value-based payment structures that reward better outcomes, allowing for more flexible integration. The lack of interoperability is another technical hurdle, as many behavioral health providers lack certified EHRs. Policy reform is urgently needed to ensure all providers can seamlessly share patient information for coordinated care.
Why is it important to manage behavioral health services with a forward-thinking approach?
A forward-thinking approach is essential to build a resilient healthcare system focused on prevention. This involves several key strategies:
- Trauma-informed care principles shift the focus to create safer, more healing environments.
- The Collaborative Care Model, which embeds behavioral health specialists in primary care teams, needs to become the standard of care.
- Mental health promotion in communities and suicide prevention initiatives are upstream solutions that build resilience and reduce the burden on the healthcare system.
As the World Health Organization notes, effective strategies require collaboration across sectors like education, labor, and justice. This forward-thinking approach isn’t just about treating illness—it’s about creating the conditions for mental wellness to flourish.
Frequently Asked Questions about Managing Behavioral Health Services
Understanding why is it important to manage behavioral health services often starts with answering common questions.
What is the difference between behavioral health and mental health?
While related, these terms are different. Mental health focuses on your emotional and psychological well-being—how you think and feel. Conditions include depression, anxiety, and PTSD. Behavioral health is a broader term that includes mental health but also examines how habits and behaviors—like substance use, eating patterns, and sleep—impact your overall health. It’s the connection between your mind and your actions.
What can a patient expect from behavioral health treatment?
Modern behavioral health treatment is a collaborative and personalized process. It typically begins with an assessment to understand your concerns and goals. Treatment often involves working with a provider to identify unhelpful thought patterns or behaviors and develop healthier coping strategies. This might include therapy, medication management, or both. The goal is not just to feel better, but to gain practical tools for managing stress and improving your quality of life long-term.
How does integrating behavioral health into primary care improve patient outcomes?
This question is central to why it is important to manage behavioral health services effectively. Integration leads to:
- Early detection: With up to 70% of primary care visits having a mental health component, issues are caught sooner.
- Increased access: Patients receive care in a familiar setting, removing barriers like stigma and scheduling difficulties.
- “Whole-person care”: Providers collaborate to create a unified treatment plan, which is crucial since co-occurring conditions can double healthcare costs.
- Better adherence: Coordinated care leads to patients being more likely to follow their treatment plans, resulting in better outcomes.
The “warm hand-off,” where a primary care doctor introduces you to a behavioral health specialist during the same visit, makes getting help immediate and seamless.
Conclusion
As we’ve seen, why is it important to manage behavioral health services is a vital call to action. Treating mental and physical health as two sides of the same coin is essential for true well-being. The benefits are remarkable: improved patient outcomes, reduced healthcare costs, increased access for diverse populations, and reduced burnout for providers.
Technology is the engine driving this change, from the accessibility of telehealth to the seamless data sharing of EHRs. However, this digital revolution must be built on a foundation of uncompromising IT security and reliability to protect sensitive patient data.
This is where Alliance InfoSystems steps in. As a Maryland-based IT services company with over 20 years of experience, we provide flexible, custom, and cost-efficient IT management and security solutions for healthcare practices. We understand the unique challenges of HIPAA compliance and safeguarding patient data. Our goal is to handle your IT, so you can focus on delivering life-changing behavioral health care.
We encourage healthcare organizations to accept integrated care models. By leveraging technology, you can secure and streamline your operations, paving the way for a future where comprehensive behavioral health care is a reality for everyone.
Want to learn how we can help your practice thrive? Explore how we can Secure and streamline your practice with specialized IT solutions for Applied Behavior Analysis.